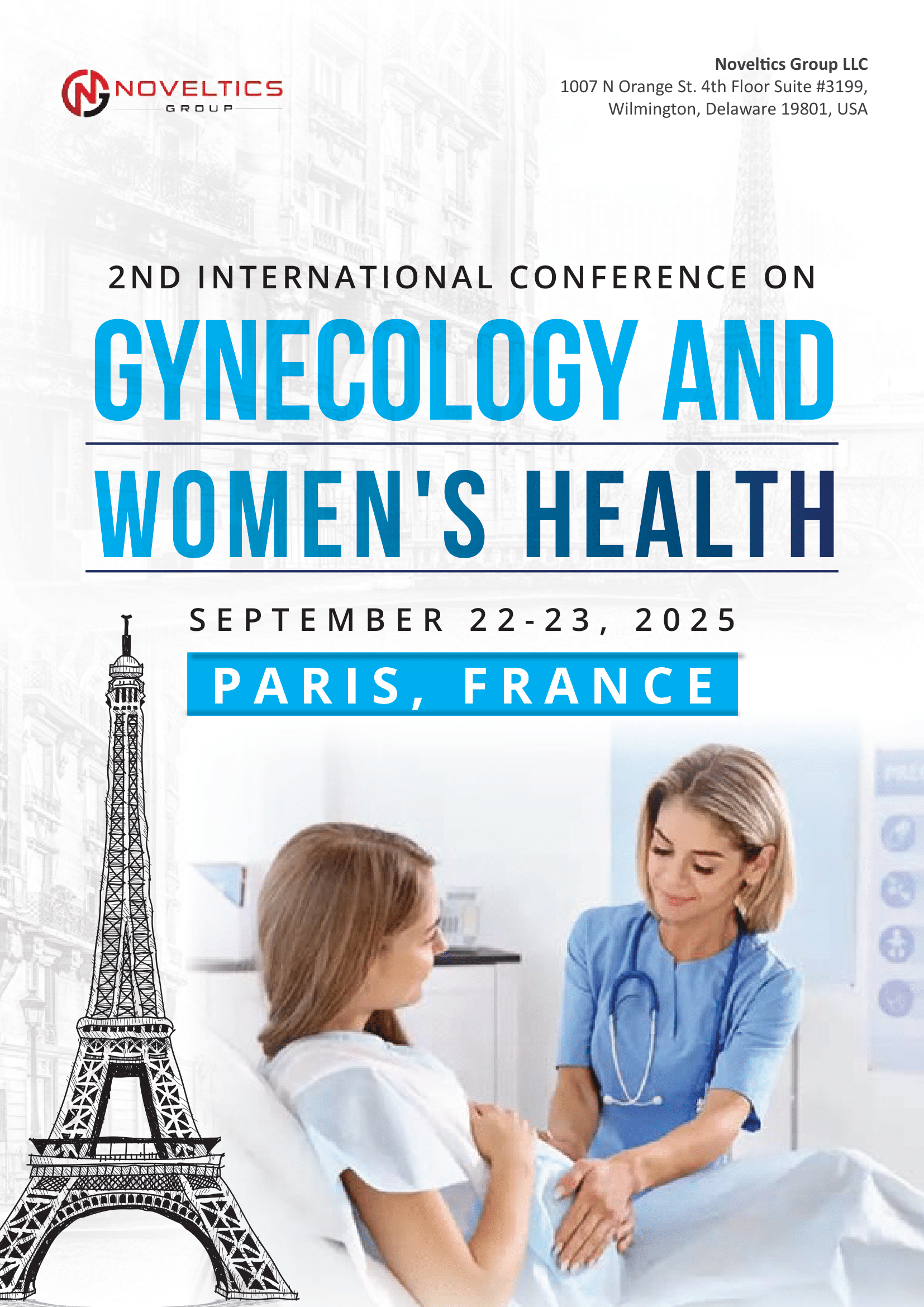
Session 01: General Gynecology
General gynecology focuses on the health of the female reproductive system, providing comprehensive care for women of all ages. Gynecologists in this field perform routine exams, screenings for conditions like cervical cancer, and manage common issues such as menstrual disorders, pelvic pain, and vaginal infections. They offer guidance on contraception, family planning, and menopausal symptoms. Through personalized treatment plans and education, general gynecologists empower women to make informed decisions about their reproductive health and overall well-being, ensuring they receive the care and support they need throughout every stage of life.
Session 02: Geriatric Gynaecology
Geriatric gynecology specializes in addressing the unique reproductive health needs of women aged 65 and older. It focuses on managing menopausal symptoms, pelvic floor disorders, urinary incontinence, and pelvic organ prolapse in older women. Geriatric gynecologists provide preventive care through screenings for cervical cancer, breast cancer, and osteoporosis, along with counseling on healthy lifestyle habits. They offer personalized treatment options tailored to each patient's needs, collaborating with other healthcare providers to ensure comprehensive care. Geriatric gynecology aims to enhance the quality of life and promote the overall well-being of older women as they navigate through the aging process.
Session 03: Gestational Diabetes
Gestational diabetes is a type of diabetes that develops during pregnancy and typically resolves after childbirth. It occurs when the body cannot produce enough insulin to meet the increased demands of pregnancy, leading to high blood sugar levels. Risk factors for gestational diabetes include being overweight, having a family history of diabetes, or being older than 25 during pregnancy. While gestational diabetes usually doesn't cause noticeable symptoms, it can increase the risk of complications for both the mother and the baby if left untreated. Management involves blood sugar monitoring, dietary changes, exercise, and, in some cases, insulin therapy. Controlling gestational diabetes is essential to reduce the risk of complications and ensure a healthy pregnancy outcome.
Session 04: Gynaecologic Oncology
Gynecologic oncology is a specialized field of medicine focused on the diagnosis, treatment, and management of cancers that affect the female reproductive system. This includes cancers of the ovaries, uterus, cervix, vagina, and vulva. Gynecologic oncologists are highly trained specialists who provide comprehensive care for women with gynecological cancers. They employ a multidisciplinary approach, collaborating with other healthcare professionals such as surgeons, radiation oncologists, medical oncologists, and pathologists to develop personalized treatment plans tailored to each patient's specific needs. Treatment options may include surgery, chemotherapy, radiation therapy, targeted therapy, and immunotherapy. Gynecologic oncology aims to improve outcomes and quality of life for women affected by gynecological cancers through advanced medical care and supportive services.
Session 05: Gynaecological Endoscopy
Gynecological endoscopy is a minimally invasive surgical technique used to diagnose and treat gynecological conditions. It involves inserting a thin, flexible tube with a camera into the pelvic cavity through small incisions, allowing visualization of the reproductive organs. Common procedures include laparoscopy for examining and treating conditions like endometriosis and ovarian cysts, and hysteroscopy for assessing and treating abnormalities within the uterus. Gynecological endoscopy offers benefits such as shorter recovery times, reduced postoperative pain, and smaller incisions compared to traditional open surgery, making it a valuable tool for providing effective and minimally invasive care to women with gynecological disorders.
Session 06: Computational Biology
Computational biology and bioinformatics play vital roles in reproductive biology by analyzing large datasets to uncover patterns, relationships, and insights into reproductive processes. These interdisciplinary fields utilize computational techniques to study genomic, transcriptomic, and proteomic data, elucidating the molecular mechanisms underlying fertility, embryo development, and reproductive disorders. By integrating computational modeling, data analysis, and experimental validation, researchers can identify potential therapeutic targets, predict treatment outcomes, and advance personalized reproductive medicine. Computational biology and bioinformatics enhance our understanding of reproductive biology, paving the way for innovative diagnostic tools, treatment strategies, and interventions to improve reproductive health outcomes.
Session 07: Pediatric Gynecology
Pediatric gynecology focuses on the specialized care of girls from infancy to adolescence with gynecological concerns. It addresses a range of issues unique to this population, including congenital anomalies, menstrual disorders, vulvovaginal conditions, and reproductive health education. Pediatric gynecologists provide compassionate, age-appropriate care and counseling, ensuring the physical and emotional well-being of young patients. Common procedures include evaluation of genital anomalies, management of menstrual irregularities, and treatment of conditions such as ovarian cysts or vaginal infections. By addressing gynecological issues early and effectively, pediatric gynecology promotes healthy development and reproductive health literacy in young girls, laying the foundation for lifelong wellness.
Session 08: Urogynaecology
Urogynecology is a subspecialty of gynecology focused on diagnosing and treating pelvic floor disorders in women. These disorders include urinary incontinence, pelvic organ prolapse, and fecal incontinence, often resulting from childbirth, aging, or other factors. Urogynecologists employ a multidisciplinary approach, integrating medical, surgical, and non-surgical interventions to address these conditions. Treatment options may include pelvic floor exercises, medication, minimally invasive procedures, or reconstructive surgery. By providing comprehensive care tailored to each patient's needs, urogynecology aims to improve quality of life, restore pelvic function, and empower women to regain confidence and control over their pelvic health.
Session 09: Nanotechnology in Gynaecology
Nanotechnology in gynecology harnesses the power of nanoscale materials and devices to revolutionize diagnosis, treatment, and research in women's health. Nanoparticles, nanosensors, and nanocarriers enable targeted drug delivery, enhancing efficacy while minimizing side effects. Nano-based imaging techniques offer superior resolution for early detection of gynecological cancers and reproductive disorders. Moreover, nanomaterials support tissue engineering applications, facilitating regenerative therapies for conditions like endometriosis or pelvic organ prolapse. By leveraging nanotechnology, gynecologists can develop innovative approaches for personalized medicine, precise diagnostics, and minimally invasive interventions, ushering in a new era of advanced care and improved outcomes in women's health.
Session 10: Women’s Health
Women's health encompasses the physical, mental, and social well-being of women throughout their lives. It addresses unique health concerns such as reproductive health, pregnancy, menopause, and conditions like breast cancer and osteoporosis. Comprehensive women's health care includes preventive screenings, contraception, prenatal care, and treatment for gynecological issues. It also emphasizes the importance of mental health support, healthy lifestyle choices, and gender-specific research and advocacy. By prioritizing women's health needs, promoting equity in healthcare access, and addressing social determinants, we empower women to lead fulfilling lives and contribute to healthier communities worldwide.
Session 11: Reproduction Biology
Reproductive biology is the study of the biological processes involved in reproduction, encompassing the development, function, and regulation of reproductive systems in organisms. It explores mechanisms of gamete production, fertilization, embryonic development, and pregnancy. Researchers investigate factors influencing reproductive success, including hormonal regulation, genetic factors, environmental influences, and reproductive behaviors. Understanding reproductive biology is crucial for addressing infertility, reproductive disorders, and contraception methods. It also informs advancements in assisted reproductive technologies, such as in vitro fertilization (IVF) and gene editing techniques. By unraveling the complexities of reproduction, reproductive biology contributes to improving fertility treatments, reproductive health outcomes, and our understanding of life itself
Session 12: Reproductive Endocrinology
Reproductive endocrinology is a specialized field focusing on the hormonal regulation of reproductive processes in both men and women. It involves the study of hormone production, release, and interaction within the endocrine system, particularly in relation to fertility, menstrual cycles, and pregnancy. Reproductive endocrinologists diagnose and treat hormonal imbalances and disorders that affect reproductive health, such as polycystic ovary syndrome (PCOS), infertility, and menopausal symptoms. Treatment approaches may include hormone replacement therapy, ovulation induction, and assisted reproductive technologies. By understanding and managing hormonal influences on reproduction, reproductive endocrinology plays a vital role in helping individuals achieve their reproductive goals and overall well-being.
Session 13: Neonatal Infection
Neonatal infection refers to the presence of harmful microorganisms in newborn infants, typically within the first 28 days of life. These infections can be acquired during childbirth, through the placenta during pregnancy, or from environmental sources after delivery. Common pathogens include bacteria, viruses, and fungi, which can cause conditions such as sepsis, pneumonia, meningitis, and urinary tract infections. Neonatal infection poses significant risks to newborns, leading to serious complications or even death if not promptly diagnosed and treated. Timely interventions, including antibiotic therapy and supportive care, are essential to improving outcomes and preventing long-term sequelae in affected infants.
Session 14: Prenatal Obstetrics
Prenatal obstetrics involves the comprehensive care and management of pregnant women and their unborn babies from conception to delivery. It encompasses a range of services, including prenatal screenings, genetic testing, and monitoring fetal development through ultrasound and other diagnostic techniques. Obstetricians provide personalized medical care, guidance on nutrition, lifestyle recommendations, and support for expectant mothers to ensure a healthy pregnancy. They also manage pregnancy-related complications, such as gestational diabetes, hypertension, and preterm labor, while prioritizing the well-being of both the mother and the developing fetus. Prenatal obstetrics aims to optimize maternal and fetal health outcomes while promoting a positive pregnancy experience for families.
Session 15: Foetal Development
Fetal development refers to the sequential growth and maturation of an embryo into a fully formed fetus during pregnancy. It unfolds in distinct stages, beginning with fertilization of the egg by sperm and proceeding through embryonic development, organogenesis, and fetal growth. During this process, cells differentiate into specialized tissues and organs, such as the heart, brain, and limbs, guided by genetic factors and environmental cues. Fetal development is orchestrated by intricate molecular signaling pathways and physiological processes, ensuring the formation of a healthy, viable offspring. Understanding fetal development is essential for monitoring pregnancy health, diagnosing abnormalities, and optimizing maternal-fetal outcomes.
Session 16: Maternal-Fetal Medicine
Maternal-fetal medicine is a specialized field within obstetrics focused on managing high-risk pregnancies through medical and surgical interventions. Its scope encompasses pre-pregnancy counseling, antenatal care, delivery, and postpartum care, with the aim of improving pregnancy outcomes and reducing complications. Maternal-fetal medicine specialists employ advanced technologies to monitor and optimize the health of both the mother and fetus.
Session 17: Menopause
Menopause marks the cessation of menstrual cycles, triggered by decreased secretion of ovarian hormones such as estrogen and progesterone. While it's a natural phase in a woman's life, individual experiences vary, leading some to seek medical advice for symptom management. Vasomotor dysfunction and vaginal dryness are consistently linked to menopause in epidemiological studies, while other symptoms like mood changes, sleep disturbances, urinary incontinence, cognitive changes, somatic complaints, sexual dysfunction, and reduced quality of life can either stem from these primary symptoms or be associated with other causes.
Session 18: Midwifery
Midwifery encompasses both a health discipline and a profession centered on women's sexual and reproductive health across their lifespan, covering pregnancy, childbirth, and the postpartum phase, which includes care for newborns. It is recognized as a medical profession in numerous countries, distinguished by its independent and specialized education, separate from the medical specialty that typically requires prior general training. A midwife is an individual dedicated to the practice of midwifery.
Session 19: Family Planning
Family planning encompasses a woman's autonomy in determining if and when she conceives, as well as her choice regarding whether to continue a pregnancy. Despite women's desires for children, the availability of family planning methods, including safe abortion and contraception, remains significantly unequal across various global regions. Integrating family planning services into maternal healthcare, especially when maternity care serves as a woman's primary interaction with the medical system, can help reduce unmet needs and promote better reproductive health outcomes.
Session 20: Reproductive Health and Fertility
Reproductive health refers to a state of overall well-being encompassing physical, mental, and social aspects concerning the reproductive system across all life stages. It entails the ability for individuals to have a responsible, fulfilling, and safe sexual life, along with the freedom to choose if, when, and how often to conceive. Human fertility is influenced by various factors including nutrition, sexual behavior, relationships, cultural norms, instincts, hormonal balance, timing, economic considerations, lifestyle, emotions, and others. Ovulation marks a woman's peak fertility period.
Session 21: Minimally Invasive Gynecologic Surgery
Minimally invasive gynecologic surgery involves the use of less invasive techniques, such as laparoscopy or hysteroscopy, to treat gynecologic diseases. Rather than a large incision, these procedures typically involve no incisions or only a few small ones. Some treatments can even be done on an outpatient basis, while others may require a short hospital stay of one to two nights. A team of surgeons collaborates to perform minimally invasive gynecologic surgery, which has been shown to reduce discomfort and shorten recovery time
Session 22: Women's Mental Health
Women's mental health involves exploring and comprehending how mental health issues impact women in distinct ways, influenced by biological, social, and cultural factors. It focuses on promoting mental well-being and addressing the prevention, diagnosis, and treatment of mental health disorders that are either unique to women or more commonly experienced by them. This field recognizes the diverse experiences and obstacles women encounter throughout their lives, spanning from adolescence to
menopause and beyond.
Session 23: Polycystic Ovary Syndrome
Polycystic ovary syndrome (PCOS) is a diverse endocrine disorder affecting approximately 6-15% of females worldwide. Characterized by hormonal imbalances and metabolic disturbances, PCOS can significantly impact women's overall health and appearance. Diagnosis typically involves the presence of anovulation, clinical or biochemical signs of hyperandrogenism, and the morphology of polycystic ovaries. Additionally, women with PCOS are at a higher risk of developing metabolic syndromes, hypertension, and cardiovascular disease
Session 24: Pregnancy and Child Birth
Pregnancy, also referred to as gravidity or gestation, is the period during which a woman carries one or more developing offspring. Multiple pregnancy indicates the presence of more than one child. Pregnancy can occur through Assisted Reproductive Technology or as a result of sexual activity. It typically spans slightly over nine lunar months, with each month approximately lasting 29 to 30 days. A child is typically born around 40 weeks after the start of the last menstrual cycle (LMP). In the initial two months after conception, the term embryo is used to describe the developing offspring; thereafter, it is referred to as a fetus until birth
Session 25: Endometriosis and Pelvic Pain
Endometriosis is a condition where tissue similar to the lining of the uterus grows outside it, causing pelvic pain, especially during menstruation. This chronic pain can also lead to discomfort during intercourse, bowel movements, and urination. The severity of pain varies, and it can impact daily activities and
fertility. Early diagnosis and treatment, including medication and surgery, are crucial to managing symptoms and improving quality of life.
Session 26: Cervical and Ovarian Cancer
Cervical and ovarian cancers are among the most common gynecologic malignancies, with early detection being crucial for improved outcomes. Cervical cancer is primarily caused by persistent infection with high-risk HPV types, while ovarian cancer often remains undiagnosed until advanced stages. Advances in screening, such as Pap smears and HPV testing for cervical cancer, and targeted therapies for ovarian cancer, have significantly improved survival rates. Ongoing research continues to focus on prevention, early detection, and personalized treatment strategies
Session 27: Nursing and Women’s Healthcare
Nursing in women's healthcare involves providing specialized care tailored to the unique needs of women across their lifespan, encompassing various stages such as adolescence, pregnancy, childbirth, and menopause. It involves promoting and maintaining women's health, preventing illness, and providing treatment and support for various gynecological and reproductive health issues. Nursing in women's healthcare also involves educating women about their health, empowering them to make informed decisions, and advocating for their rights and well-being within the healthcare system.
Session 28: Advancements in Gynaecology and Obstetrics
The prevalence of obesity among adult women and teenagers is increasing, contributing to a rise in the number of cesarean deliveries. Advances in women's health also encompass increased genetic testing, awareness about zakat and dengue contagion, the association between preeclampsia and stroke-related deaths, the effects of cannabis use, and the evolution of obstetrics. Obstetricians and gynecologists should possess the appropriate skills, knowledge, and techniques to conduct comprehensive examinations, including assessments of the neck, chest, bones, abdomen, and lower extremities, for both pregnant and non-pregnant women.

.png)


















.png)
.png)




.png)














"Hello, my name is Dayo Princeton Oladipo. I'm from Berlin, Germany. I arrived here in Paris at the conference, and I'm the CEO and co-founder of AREWA health with Dr. Oyedupe O. Gläsmann. And we document and assist doctors with medical reports to determine pathological values during pregnancy and afterwards send them over to the pregnant woman."